In a modern glass and steel building, embedded in the Burnside Industrial Park,
The
The pathology building has a similarly vibrant atmosphere, despite its purpose. The office is shockingly normal, given
Matthew Bowes and his team of forensic pathologists and nurse death investigators use
Forensic nurse Lindsay Denis pulls her long blonde ponytail over her shoulder and begins to run her fingers through it while thinking back over the cases she’s worked. Just over a year in, she’s still new to the team.
“The worst part and the best part are the families,” she says. “You know, I had that baby.”
Shauna Curley leans over and pats her arm, and Eveline Gallant smiles encouragingly. Both of Denis’ co-workers have been with the province’s forensic pathology team for many years, veterans of the morbid, gory and tragic.
“We got a call about a deceased infant. I went to pick up the body—poor thing was only a few months old,” says Denis. “We normally don’t do visitations or viewings. We’re not set up for that. But something about this really pulled at me. I went to talk to
Forensic nurses deal with what Curley calls the “golden triangle of death”: The scene, the autopsy and the deceased’s medical history.
When a body is found or a death occurs, a phone rings in the ME’s office. One of the forensic
The office handles all cases that are criminal, suicide or unexplained natural deaths. Curley, for instance, was on the frontlines of the Swissair tragedy in 1998, when a flight bound from New York to Geneva crashed into the waters off Peggys Cove, killing all 229 aboard.
Whichever forensic nurse is tasked on the day to go out to the scene takes the phone next and begins
The forensic nurse is then dispatched to the death scene. They’ll sort through the deceased’s belongings, hunt through medicine cabinets and dig through garbage cans, looking for clues to explain the cause of death. When the scene is processed, the body is brought back to Burnside for the ensuing autopsy.
Bowes, who has been chief medical examiner since 2006, did his fellowship
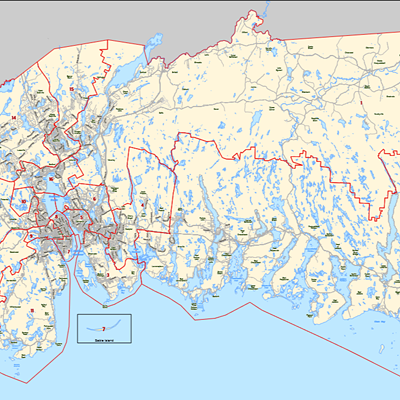
Prior to the centralization, autopsies in this province were done in whatever hospital was close enough to the body’s discovery site. Family doctors and other general practitioners would be called to perform the procedure and collect specimen samples. It was a logistical nightmare for the medical examiner’s office to orchestrate during the best of times.
The marriage of these two archetypes—forensic nurse death investigators and a consolidated headquarters—is the system Nova Scotia has in place today: A
The morgue in the
It’s here where the bodies are brought for
Each autopsy takes about 45 minutes to an hour. The team has it down to an exact science. There’s no wasting of time, no indignity and no malice—just a job to do.
“There’s this misconception that autopsies are mutilating, and that’s just not true,”
Bowes says, through his surgical mask, as he preps for the next case.
Four people and five bodies partake in the process. The technician and the medical examiner are the one’s doing the “cutting,” and so wear latex aprons that have the unfortunate fashion design of making the individual look like a giant Lego block of dark teal.
Then there is the “float,” who will be acting as the go-between in the lab—getting instruments, answering the phone and filling in paperwork.
The final staff member in attendance is the forensic photographer, who begins taking photos from crown to
Bowes (or whoever is the attending doctor that day) examines the exterior of the deceased, looking for bruises, cuts, scrapes, tattoos, scars and other identifying features.
Then the technician begins the infamous Y incision: Take your pointer finger on each hand and touch it to your upper chest where your collarbone meets your shoulder. Draw a line diagonally towards the middle of your chest until your fingers meet on your sternum (the central bone segment that melds your ribs together and protects your internal organs), then drag both pointer fingers down in a straight line to your belly button and then past the waistline of your pants to just above the groin region. That’s the size of the standard Y incision.
Moments later, the body has two wings of tissue folded away from its torso, exposing the ribcage and intestines. The intestines are removed first and put directly into a pink plastic bag that’s kept to one side. Red-handled garden shears carefully snip the ribs around the sternum. They make a distinct wet crunch as they’re cut.
“You would be surprised how often we get our instruments from Canadian Tire,” says one of the attending nurses. “Any medical supply store marks up the price if it says the word ‘forensic’ on it.”
Blood, urine and vitreous fluid—found in your eye—are collected as samples for toxicology reports. The core torso organs are extracted and put into a stainless steel bowl, where they will be separated, weighed, cross-sectioned and deposited into another pink plastic bag.“People ask me if I am sad that I am not in nursing anymore. I tell them that I am, my patients just aren’t living.”
tweet this
Bowes begins examining the liver, which in this case has evidence of cirrhosis—small yellowish nodules are visible on the surface. Using what resembles a long cake knife, he carefully slices into the organ and separates the cuts on a white plastic cutting board. He points to the grease that appears on the knife blade, evidence of a fatty liver.
Each organ goes through the same process: Rinse, slice, assess and repeat.
The brain requires a bit more work. Carefully placed incisions around the back of the head allow the skin to be pushed down away from the skull. The whine of the bone saw fills the morgue and within minutes, a large section of skull is skillfully removed from the base. Sharp taps from
Slivers of the other critical organs are placed in pink “cassettes” (a small grid-patterned plastic case) and larger pieces in a “stockpot” of formalin to be examined even further at the IWK.
The wonder of the human body doesn’t escape Bowes as he performs his work, regardless of his years of experience and exposure to death. He smiles over cross sections of the heart.
“Look at these,” he says, pointing at the heart’s valves, the awe in his voice unmistakable. “These slap together almost 70 times a minute for 80 years.”
Finished with the cross-sections of the organs, he carefully packs them up in the pink bag by his elbow. Then the process of preparing the body for pick-up begins.
Baby-blue absorbent pads are placed in the torso to soak up remaining blood and fluids. The same pads are carefully folded into the skull cavity to mimic the space the brain would have taken up.
While the stations are wiped down, the technician threads a curved needle with waxed twine that hangs from the ceiling on a spool. A loose corset is laced along the front of the torso, preparing the body for its trip to the funeral home.
Taking Ivory soap and some green-and-yellow Scotch-Brite sponges, the technician washes down the corpse—tenderly and efficiently wiping away any blood and grit from the scene until both body and morgue gleam under the lights. The team is ready for its next patient.

Back in the lunchroom outside, Lindsay Denis takes a sip from her grey plastic water bottle and settles into the rest of her story. The dead child’s mother and father were brought into building’s private “grieving room,” she says, where families are usually told the results of an autopsy. Denis had to explain how their baby’s body would look normal, but not alive—blue and cold.
“I can just remember sitting in that chair, having to supervise them and watching them sob hysterically over this dead baby,” Denis says. “I just kept staring out the window and repeating to myself ‘This is not mine, I do not own this,’ and focusing on what a beautiful day it was outside.”
The cell phone on the lunch table next to Shauna Curley’s hand is buzzing incessantly, even as her co-worker recites her sombre anecdote. It’s one of the certainties in this workplace: The phone will always ring. Death is never kept waiting.
“People ask me if I am sad that I am not in nursing
It’s a sentiment echoed by Bowes. His team provide closure for families suffering from not knowing what happened to their loved ones. The forensic pathology team might work with the dead, but what they offer is medicine for the living.
“If I am able to tell a grieving mother the reason her child died was not from something she did, that there was nothing she could do to save him, I’ve made an incredible difference in her life,” he says.
“This is the most important job in the world.”